PREIMPLANTATION GENETIC DIAGNOSIS FOR BRCA 1/2 CARRIERS
A
Assisted Embryo Hatching
a procedure in which a hole is made in the zona pellucida of the early embryo. The embryo may more easily “hatch” out of the zona through the hole prior to implantation.
Assisted Reproductive Technologies (ART)
a collective term which refers to a variety of medical procedures used to achieve pregnancy.
B
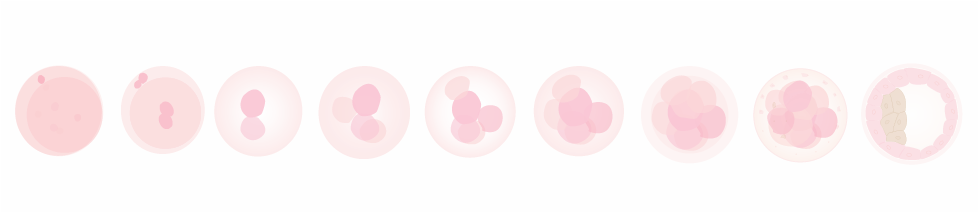
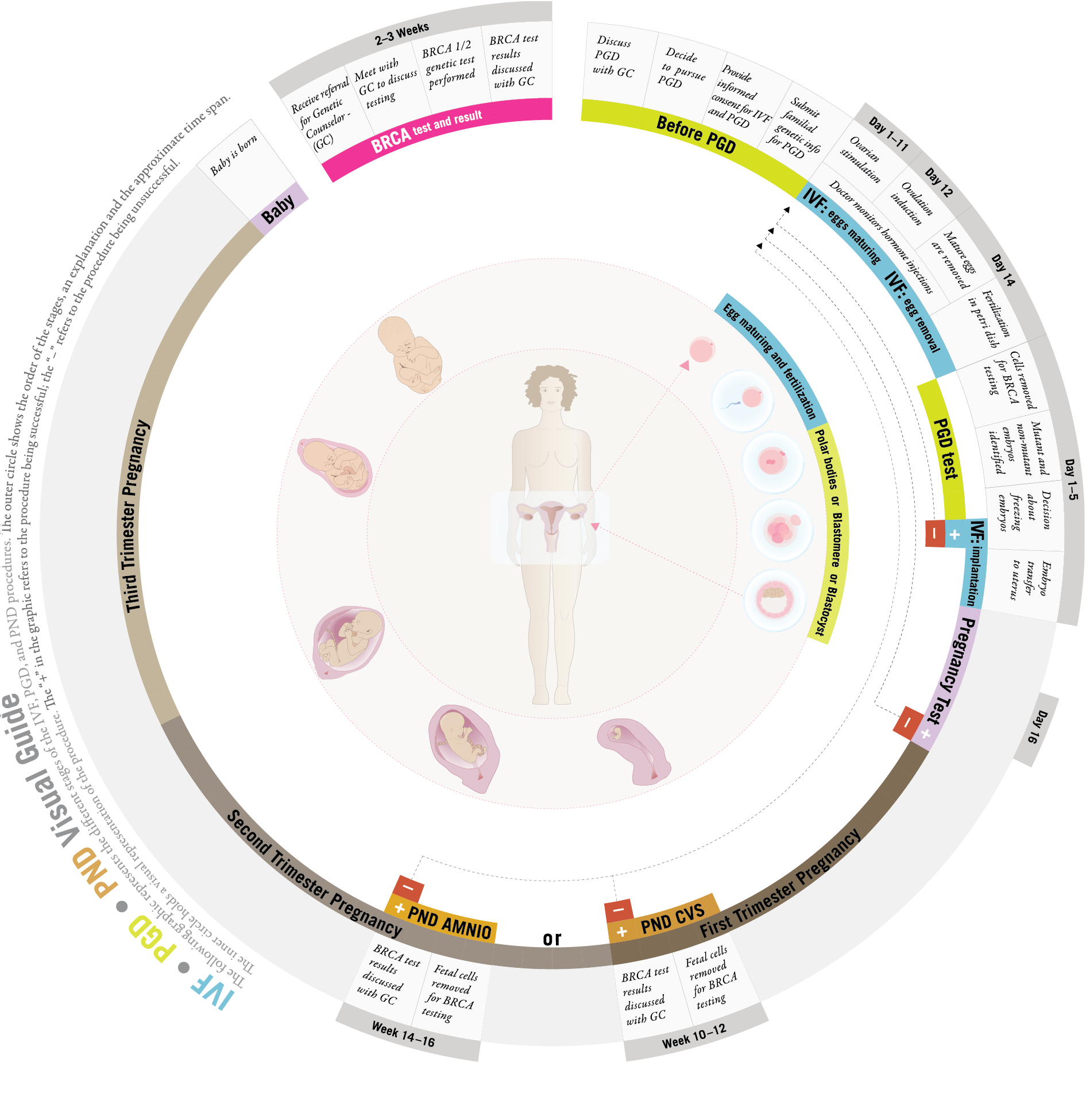
Blastocyst
the stage of development that the embryo is in when it enters the uterine cavity for implantation (typically 5-6 days after fertilization). It is comprised of two types of cells; an outer layer of cells called the trophoblast that will become the supporting tissue of the embryo such as the placenta and an inner layer referred to as the Inner Cell Mass, which will be multiply and contribute to the cells of the embryo.
Blastomere
a single cell from the developing 3-day embryo.
C
Cryopreservation
halting the embryo development before implantation through a freezing procedure.
Controlled Ovarian Hyperstimulation (COH)
the use of medications to stimulate growth and development of multiple ovarian follicles.
F
Follicle
a structure in the ovary that has nurtured the ripening egg and from which the egg is released or retrieved.
Follicle Stimulating Hormone (FSH)
a hormone produced by the pituitary gland that stimulates the ovary to ripen a follicle for ovulation.
Fluorescent in-situ hybridization (FISH)
a type of visualization used to determine the chromosome number and chromosomal mutation status of the embryo via PGD or PND.
G
Genetic counselor
a medical professional with specialized training in clinical genetics.
I
Intracytoplasmic Sperm Injection (ICSI)
an assisted fertilization technique in which a sperm is micro injected directly into the egg cytoplasm.
In Vitro Fertilization (IVF)
a procedure during which an egg is removed from a ripe follicle and fertilized by a sperm outside the human body.
L
Linkage Analysis
involves the study of BRCA1/2 inheritance patterns within a family and the identification of genetic markers that map near the gene. These genetic markers are physically linked to the gene.
M
Meiosis
this term describes cell division that occurs during the formation of the mature egg and sperm. During meiosis, the number of chromosomes (genes) is reduced so that the egg and sperm contribute only half of the parent’s genes to the embryo.
O
Ovarian Hyperstimulation Stimulation Syndrome (OHSS)
a medical complication of the stimulation procedures and medications in which stimulated follicles produce excess hormones and other factors which may lead to serious complications and may cause cancellation of a cycle and for a small number of women may result in death.
P
Polar body
a polar body is a small cell that is naturally released by the egg or oocyte during the process of meiosis. The first polar body is released by the oocyte near the time of ovulation. The second polar body is released by the oocyte, at the time of fertilization. The polar bodies do not contribute to the developing embryo, but are naturally discarded by the oocyte during the process of meiosis. Because the polar body contains one half of the possible genetic information of the mother, the genetic information of the oocyte can be inferred by the genetic testing of the polar body.
Polymerase chain reaction (PCR)
one of the most widely used laboratory techniques for visualizing genetic information and can be used for PGD or PND.
Preimplantation Genetic Diagnosis (PGD)
refers to procedures that are performed on embryos prior to implantation, sometimes even on oocytes prior to fertilization to determine gene status.
Prenatal Diagnosis (PND)
testing for genetic mutations in a fetus during the first or second trimester of pregnancy.
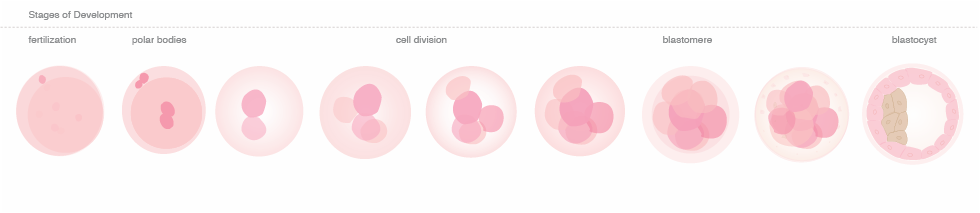
A Visual Guide to BRCA and PGD:
The following graphic represents the different stages of the IVF, PGD, and PND procedures. The outer circle shows the order of the stages, an explanation and the approximate time span. The inner circle holds a visual representation of the procedure.
The "+" in the graphic refers to the procedure being successful; the "–" refers to the procedure being unsuccessful.
Introduction:
If you are reading this web page, it is likely that you have a family history of breast and/or ovarian cancer and have undergone genetic testing for mutations in the BRCA1 or BRCA2 genes. As you may know, individuals with mutations in these genes have an increased lifetime risk of developing breast and ovarian cancer as well as certain other forms of cancer. (info 1)
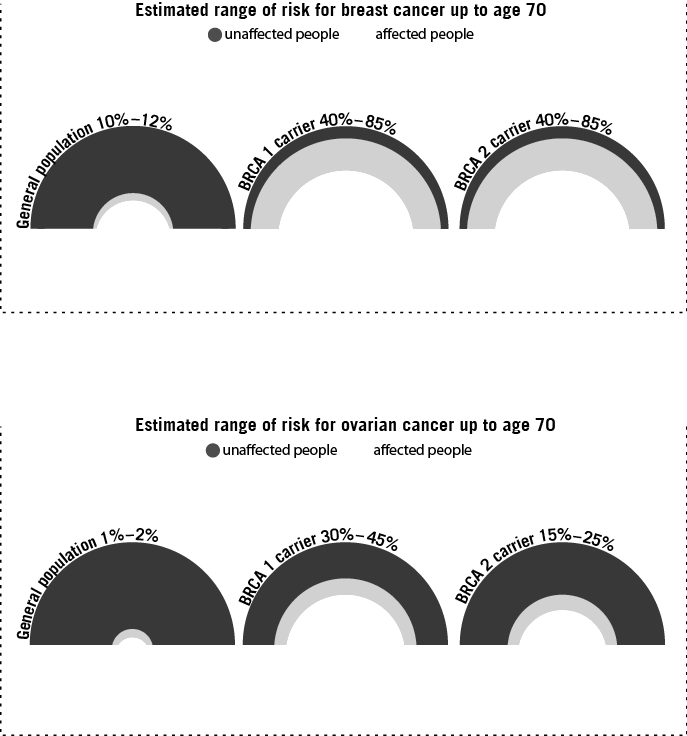
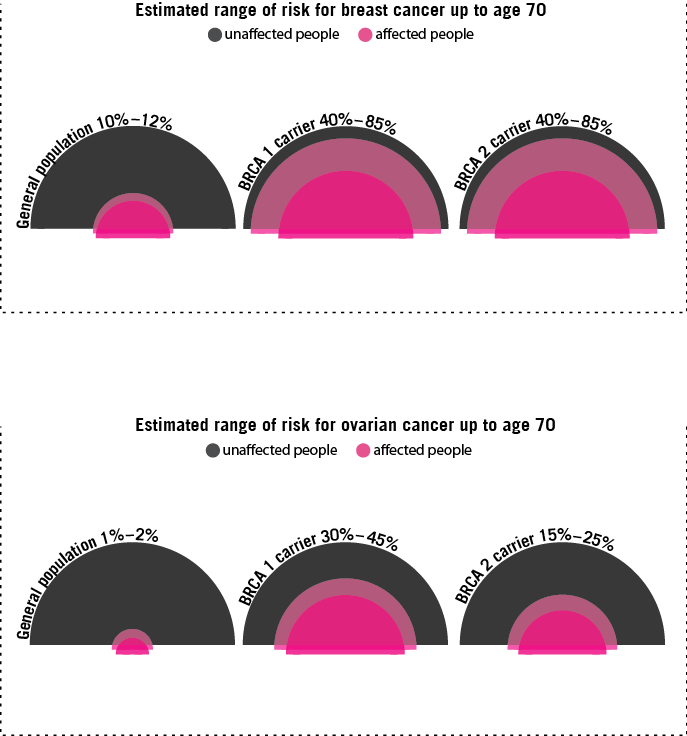
Info 1: Estimate risk of breast and ovarian cancer up to age 70
Estimated risk of developing cancer varies as it is based on many different models to predict risk. Not all models apply to all patients. Each model is appropriate only when the patient’s characteristics and family history are similar to the study population on which the model was based. In addition, other factors may increase or decrease a person’s risk relative to this range, and risk will increase with age.
PGD involves a genetic test that screens embryos for the presence of genetic mutations before pregnancy. PGD has been used since 1990 to detect genetic mutations and chromosomal abnormalities that lead to early childhood death or defects in cognitive development. More recently, PGD has been used to screen for gene mutations associated with increased cancer risk, including BRCA1/2.
The use of PGD for BRCA1/2, is different than some conditions for which PGD is more commonly used because 1) only a proportion of carriers will go on to develop cancer; 2) onset of disease occurs later in life and is sometimes treatable; and 3) there are cancer risk reduction methods including early surveillance and prophylactic measures.
Knowing your carrier status means you have more information about your personal risk profile than most. Through the help of a cancer doctor and genetic counselor you can use this information to find the best plan for management of your individual risk.